Stress, Chronic Stress and IBS
Lin Chang, MD, Professor of Medicine, Oppenheimer Center for Neurobiology of Stress
April is IBS Awareness Month. IBS, or irritable bowel syndrome, is one of the most common gastrointestinal (GI) conditions diagnosed in primary care and gastroenterology practices. Multiple factors, including a family history of IBS, prior GI infection (e.g. food poisoning), and stressful life events contribute to the development of IBS. The role of stress in health and disease is a particularly relevant topic in these unprecedented times of the COVID-19 pandemic. Life has changed for all of us and will likely change forever to some extent.
Effects of Acute and Chronic Stress
Stress is a complex concept. Stress can be acute (short-lived) or chronic (prolonged) and range from daily hassles to life-threatening situations, such as natural disasters and violence, that trigger the “fight or flight” response. Our body responds to acute stress differently than it responds to chronic stress. For example, during an acute stressor, our immune response can increase, pain sensitivity can decrease and certain types of memory can improve. Chronic stress can have the opposite effect. It can increase pain sensitivity and negatively impact memory and mood. Over time, chronic or recurrent stress results in an increased demand on our bodily systems.
Allostatic Load
The wear and tear on the body, termed “allostatic load,” set in motion long-term patterns in behavior, physiological reactivity, and other changes that can lead to disease and health-damaging behaviors, e.g. drug dependence. Chronic overactivity or under-activity of allostatic (or adaptive) systems occurs. Allostatic systems include the cortisol response, autonomic nervous system (the sympathetic “fight or flight” system and the vagal or parasympathetic system), and cardiovascular, GI, metabolic, and immune systems. Allostatic load clinically presents as fatigue, irritability, muscle aches, and feelings of demoralization as well as GI symptoms including abdominal pain, diarrhea, or constipation, which are the key symptoms of IBS.
Stressful life events and IBS
Increasing scientific evidence shows that IBS is a stress-sensitive condition. In predisposed individuals, sustained stress can result in persistent, increased responsiveness of the central stress response and vulnerability to develop IBS. The role of stress may be particularly important in altering the way the brain and gut communicate, which affects gut function, and this change can result in the development and/or flare of IBS symptoms. Significant stressful life events that occur in childhood and/or adulthood can increase the risk of having IBS. Adverse childhood experiences, such as verbal, sexual and physical abuse, and mental illness of a parent increases the risk of having IBS. However, this association is not specific to IBS. Large-scale studies have shown that adverse childhood experiences increase the risk of multiple chronic illnesses including chronic heart or lung disease, diabetes, obesity, and substance abuse. Confiding in others about the traumatic event at that time can reduce the risk of developing IBS. Here is one example of how this can be accomplished: https://romedross.video/ChangTopics . Experiencing stressful life events in adulthood also increase the risk of IBS, the severity of symptoms, and reduce the quality of life. Once a patient develops IBS, stress can trigger symptom flares.
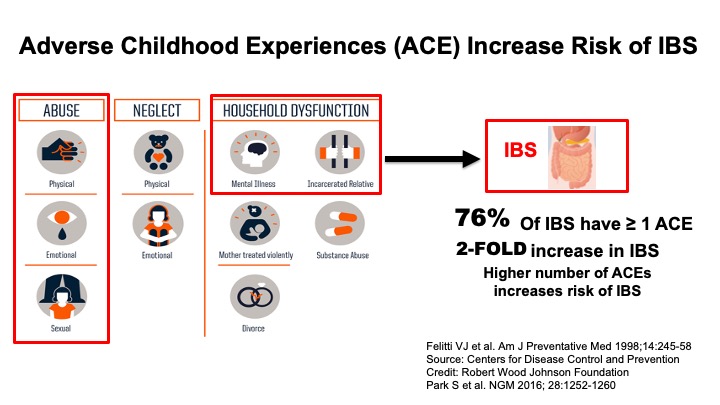
• The ACE Study: >17,000 Kaiser members
• Independent dose response effect between number of EALs by ACE and negative health outcomes
The Future of IBS and Stress
Understanding the biologic mechanisms of stress hyper-responsiveness in IBS patients may help identify a biologic diagnostic test or targets for future treatments. In addition, recognition of stress-related IBS symptoms can help guide management approaches, including earlier and more effective treatment interventions to reduce the risk of developing IBS or reduce the symptoms in those with IBS. These treatments include comprehensive stress management, behavioral therapy, and resilience training programs.
