Acupuncture Treatment for the Disorders of Gut-Brain Interaction (DGBI) A Report from China
Written by Xiucai Fang, MD – Peking Union Medical College Hospital, Beijing and Jianbin Zhang, MD – Nanjing University of Chinese Medicine, Nanjing
What is Acupuncture?
Acupuncture is a treatment method, which ancient Chinese doctors have used for more than two thousand years. It is widely used in Chinese medicine as there are designated acupuncture departments in traditional Chinese medicine hospitals. Also, there are many practitioners in the Chinese medicine departments in general hospitals. It has affected and spread to more than 100 countries and regions around the world. Acupuncture uses specific tools (the most commonly used form is stainless steel needles) to place on specific parts of the human body surface, and it produces local effects, distal effects, and even systemic effects to achieve the purpose of preventing and treating diseases.
Which Diseases Are Suitable for Acupuncture Therapy?
Of the 64 disease indications published by the WHO organization, acupuncture has been identified as being of value in treating pain disorders and digestive tract diseases ([especially for disorders of gut-brain interaction, DGBI], previously called functional gastrointestinal disorders) and reproductive problems. It is a complementary and alternative medicine (CAM).
Are There Differences Between Manual Acupuncture and Electroacupuncture?
Two forms of acupuncture manipulation used clinically are manual acupuncture (MA) and electroacupuncture (EA). In MA, the acupuncturist inserts the needle into a specified acupoint located beneath the patient’s skin. Then, after reaching the required depth, needle manipulation techniques such as lifting and thrusting and/or rotation are applied. For EA, the acupuncturist inserts the needle into a specified acupoint, and then the needles are connected to the electrical stimulator to provide electrical pulse stimulation to the acupoints. Generally speaking, MA requires the operator to have more experience. It also permits individualizing therapy, i.e., specifically tailored acupoints are used according to the patient’s condition, and modifying handle needle lifting and thrusting, needle rotation, and the speed of each patient, respectively.
Is the Acupuncture Therapy Effective on DGBI?
More and more studies have shown that acupuncture and other complementary and alternative medical practices are an efficacious method in treating DGBI, including functional dyspepsia (FD), irritable bowel syndrome (IBS), and functional constipation (FC).
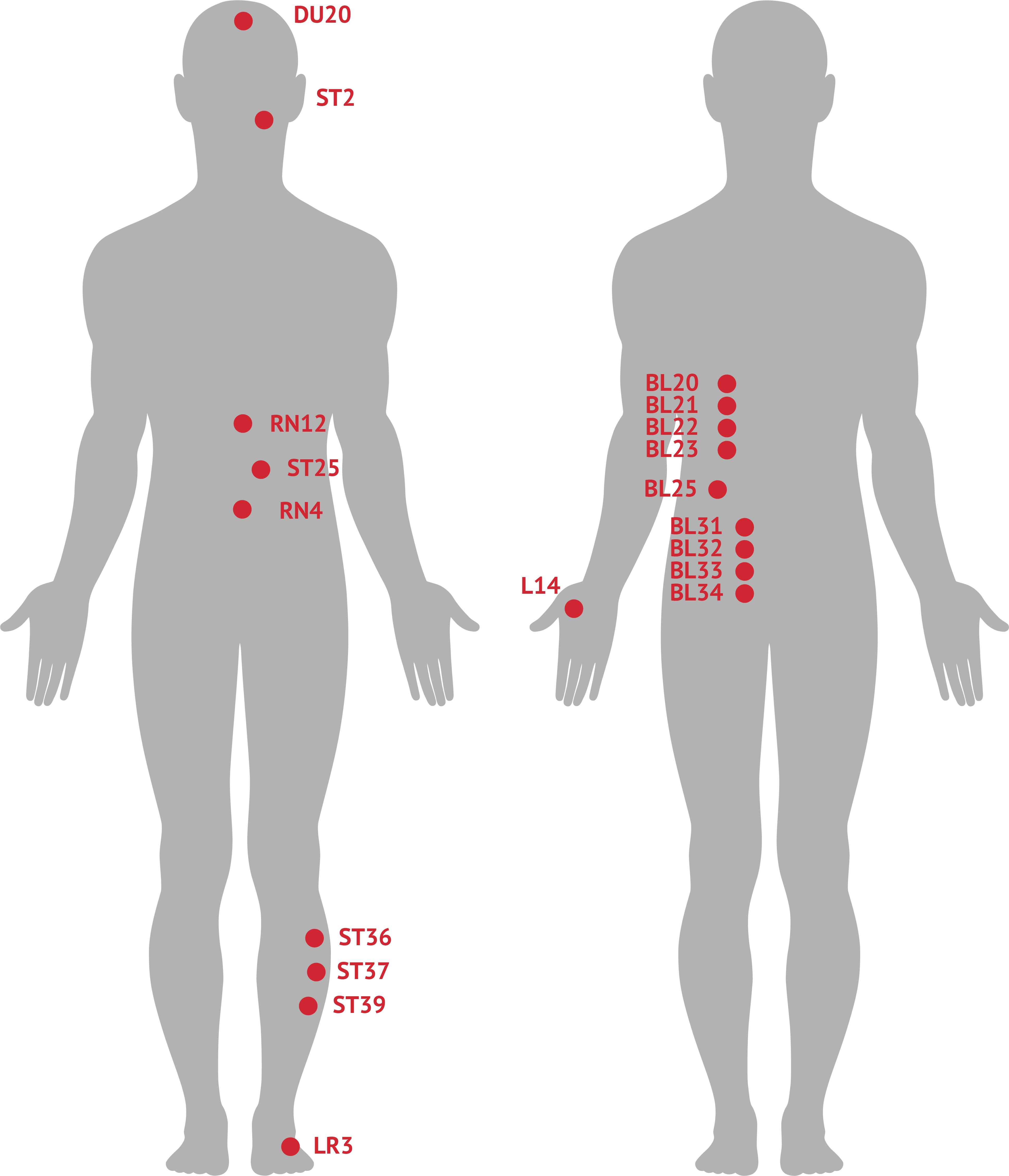
In FD patients, acupuncture treatment can improve their dyspeptic symptoms, including postprandial discomfort, early satiety, upper abdominal pain, upper abdominal burning pain, belching, abdominal fullness, and distention in most patients. One study enrolled 76 FD patients, who were randomized into the acupuncture group and the control group. In the first four weeks, the acupuncture group received individualized acupuncture treatment (standard acupoints and the selection of points according to symptoms). The control group awaited acupuncture treatment, and during the following four weeks, received acupuncture. The results showed that the acupuncture treatment in the first 4 weeks was enough to alleviate the patients’ symptoms, such as abdominal pain, upper abdominal burning, and postprandial satiety, and the effect lasted for 8 weeks after treatment. Acupuncture is also effective in improving the patients’ mental and emotional state and quality of life with refractory functional dyspepsia. Acupoints for the treatment of FD include Zusanli (ST36), Zhongwan (RN12), Pishu (BL20), Weishu (BL21), Sibai (ST2), and Neiguan (PC6). (See Figure 1).
Patients with IBS usually present as recurrent abdominal pain associated with a change in stool frequency and appearance. For patients with IBS-D, EA is equal in reducing defecation frequency and has fewer adverse events than loperamide. A comparative effectiveness systematic review and meta-analysis of Chinese trials reported more significant benefits from acupuncture than pharmacological therapies. Acupuncture can improve the symptoms of pain, anxiety, and depression in patients with IBS. Acupuncture could likely be more effective for refractory patients when used as a component of integrative treatment. The acupoints for the treatment of lBS include Baihui (DU20), Hegu (LI4), Taichong (LR3), ST36, Tianshu (ST25), Guanyuan (RN4), BL20, BL21, Sanjiaoshu (BL22) (see figure 1).
FC is the most common DGBI in the general population worldwide, which presents as infrequent, incomplete and difficult defecation. There is strong evidence of the effectiveness of acupuncture in FC treatment, including increasing defecating frequency, reduced difficulty in defecating, and improved quality of life. After eight weeks of EA treatment, the proportion of FC patients with three or more mean weekly complete spontaneous bowel movements (CSBMs) reached 31.3% and 37.7% over the treatment and follow-up periods until week 20, respectively, compared with 12.1% and 14.1% in the sham EA treatment. The acupoints used to treat constipation include ST25, Shangjuxu (ST37), BL22, Shenshu (BL23), Dachangshu (BL25), Shangliao (BL31), Ciliao (BL32), Zhongliao (BL33), Xialiao (BL34) (see figure 1).
How Long Should Be Took for Acupuncture Therapy?
The recommendation for the frequency and duration of acupuncture treatment, is 3-5 times a week for 4-8 weeks. For patients with severe conditions, increase the treatment time as appropriate, and in general increase or decrease the treatment time, according to the patient’s condition.
Is the Acupuncture Safe?
Acupuncture is a safe therapy with a low risk of adverse events.
Figure 1. Acupoints of acupuncture therapy for DGBI